What does “biliary” mean?
“Biliary” refers to the system of ducts that drain bile from the liver to the intestine. Bile is a tacky yellow-green fluid that is made by the liver. It is either temporarily stored in the gallbladder on its way to the intestine, or it passes through the bile ducts directly into the intestine where it aids digestion. If there is a blockage and bile cannot drain out of the liver it collects in the body and causes the skin to turn yellow (jaundice), the white part of the eyes to turn yellow (icterus), the urine to turn dark brown, and the stool to become pale brown. Most patients with jaundice have itchy skin. Other symptoms include nausea and poor appetite. If the bile becomes infected it can cause sepsis (blood infection) for which a biliary tube can drain the bile, relieve the infection, and be life saving.

What is a biliary tube?
It is a small plastic tube that is inserted through the skin, across the liver, and directly into the bile ducts (as you can see in the cartoon image). It drains bile outside the body into a bag, or the tube may cross the blockage and allow bile to enter the duodenum, in which case an external bag may not be necessary.
Why do I need a biliary tube?
You have a blockage (obstruction), or leakage, somewhere in the biliary system. The most common reasons for this are:
-
Stones
-
Cancer/tumor
-
Prior surgery that can cause scarring (obstruction) or internal leakage of bile.

Your doctor may have recommended for you to have a cholangiogram (image guided procedure of the biliary system) to assess for a biliary drainage catheter placement. This will allow the bile to drain from your liver.
There are 3 different ways bile can be drained from your liver.
-
An external biliary drainage catheter goes through your skin and into your bile ducts. It will be placed above the blockage. After this procedure you will have a catheter coming out of your body, attached to a drainage bag.
-
An internal-external biliary drainage catheter goes through your skin and into your bile ducts, across the blockage. One end of the catheter will sit in your small intestine, and the other will come out of your body and will be attached to a drainage bag. This catheter lets bile flow in 2 directions, either out to the external collecting bag or into your small intestine. This is the most common kind of drainage catheter, but not everyone is able to get this type.
-
Internal biliary drainage (stenting) uses a metal cylinder (called a stent) to hold the blocked area open. After this procedure you may have a small catheter coming out of your body. If you have a catheter, you will have a follow-up procedure in 1-2 weeks to see if the stent is working well. If it is, the catheter will be removed.
If you had a drainage catheter placed, it will be attached to a bag to collect the drainage. Your doctor will give you an idea of how much drainage you should expect.
How is a biliary drain placed?
Your procedure will be done at El Camino Hospital where you will be set up with an IV to allow access for moderate, also known as “twilight” sedation, or general anesthesia. You will then be taken to the procedure room where you will have a team of two nurses, a radiology technician and your interventional radiologist. You will be connected to heart, blood pressure and oxygen monitors during the entire procedure. IV medication will be administered to make you comfortable (moderate sedation). Using x-ray (fluoroscopy) guidance, your liver is visualized. A site on the skin of the produral area is cleaned and sterilized and local anesthetic is injected in this area to numb the site. Then a small needle is inserted through the skin and into the biliary duct. A guide wire is then placed and maneuvered into position, replacing the needle. Once in good position, a small drainage catheter (biliary tube) is then slid over the guidewire, replacing it. A cholangiogram is then performed where a small amount of contrast material (dye) is injected to “map” out the biliary system and identify the area of blockage or leakage. Once identified, depending on the extensiveness of the problem you will get either an external biliary drain or internal-external biliary drain placed. The biliary drain is then anchored in place using a small suture on your skin and attached to a drainage bag. This procedure takes about 30-60 minutes.

What can I expect after the procedure?
You will recover after your procedure for about 1-2 hours where your procedure site, heart rate, blood pressure, and oxygen saturation will be monitored. Your family will be able to see you soon after the procedure in the post-operative area and you will be able to eat and drink once you are awake and able to. You should expect to have some mild tenderness and discomfort at the biliary drain site for the next 2-3 days.
How often should I change the Biliary bag?
The bag only needs to be changed when it gets dirty or smells bad. It is variable, but for most patients the bag should be changed every 2 weeks.
Where can I get new bags?
You should receive an extra bag before you leave the hospital after the insertion of the biliary tube. When you come to your follow up appointment we can give you an additional bag, if needed.
Bile drainage bags can also be bought at a medical supply store.
MOUNTAIN VIEW:
CAMINO PHARMACY
701 E. El Camino Real – 2nd floor
NOREL PROSTHETICS
205 South Drive
P: 650.934.7699
P: 650.968.7464
FREMONT:
HALLERS PHARMACY
37323 Fremont Blvd
P: 510.797.2772
PALO ALTO:
PALO ALTO ORTHOPEDIC
3910 Middlefield rd
P: 650.813.9300
SAN JOSE:
SANTA CLARA OSTOMY AND MEDICAL
2455 Forest Ave
BISCHOFF’S MEDICAL SUPPLY
225 North Bascom Ave
P: 408.296.7890
P: 408.286-6651
SANTA CRUZ:
HORSNYDER PHARMACY
1226 A Soquel Ave
P: 831.423.2315
SAN FRANCISCO:
BISCHOFF’S MEDICAL SUPPLY
1635 Divisadero st. #105
P: 415.921.0440
When should I flush the biliary tube? How do I do it?
You only need to flush the tube if:
-
There is no drainage in the biliary tube. This may mean that the tube is clogged.
-
There is a significant amount of blood in the tube such that the tube will likely get clogged.
Most patients should flush their drains daily. This will keep the drain from becoming clogged (with re-accumulation of fluid in the body and ultimately delaying removal of the drain). Learning to flush the drain takes some simple training, but once you understand the procedure it is easy and takes 5 minutes. You must take a small syringe ( 5 – 10 ml ) and fill it with sterile water or saline. There should be a 3-way stopcock in the line between the drain and the bulb.
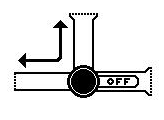
The syringe fits on the side port and the stopcock is rotated into different positions to flush toward the bag or biliary tube.

In this position you CANNOT inject from the sideport. This is the position for flow from the biliary tube to the bag. The stopcock should be in this position unless you are flushing the line.

In this position you CAN inject from the sideport. This will clear the biliary drainage tube.

In this position you CAN inject from the sideport. This will clear the line into the bag.
How to empty the bag?
-
Wash your hands well with soap and water.
-
Find the drainage valve at the bottom of the bag and turn the valve to open.
-
Drain the fluid into the commode. Write the amount of your drainage and the date and time you collected it on a drainage chart.
-
Turn the valve to the closed position.
-
Wash your hands when you are done.



How to care for the skin and the catheter site?
-
Wash your hands well with soap and water.
-
Remove the dressing from around the catheter. Use soap and water or saline or peroxide on a gauze pad/cotton pad. Clean this area once a day.
-
When the catheter site is clean and dry, place a new dressing around the drain. Put surgical tape on the dressing to hold it down against your skin.
-
If it is bloody, wrap it in a small plastic bag. Place the old dressing into the trash.
-
Wash your hands.
How long will the biliary tube stay in place?
It will stay in place as long as necessary. In rare cases they can even stay for years. Alternatively, in some patients a BILIARY STENT can be placed. This is a plastic or metal mesh tube that keeps the bile duct open and permits bile to drain to the intestine.
When should you call your physician?
-
Fever or chills > 101.5 F
-
Worsening of redness or worsening of pain in the procedure area
-
Significant bleeding for >24 hours
-
If the drain gets clogged.
-
If the drain gets accidentally removed.
-
If there is leakage around your drain
You can reach your Interventional radiologist at 650-404-8446
General Instructions:
Sedation
-
If you received sedation, you should not drive, consume alcohol, operate heavy machinery or make any important decisions for the remainder of the day.
Activity
-
You may resume your regular activities (including driving) after 24 hours unless you have been restricted for another reason.
-
No exercising, lifting heavy objects or strenuous activity for the next 24 hours.
Pain Management
-
You may use over-the-counter non-steroidal anti-inflammatory drugs (NSAIDs) such as Acetaminophen (Tylenol) or Ibuprofen (Advil /Motrin) for minor discomfort, unless you are restricted from taking these medications.
-
For more severe pain, we will prescribe a narcotic medication such as Norco.
-
You should also take Colace (stool softener) daily while taking the narcotic medication to prevent constipation, which is a common problem while taking these medications.
Diet
-
You can resume your normal diet. Some patients may develop nausea after the sedation. Therefore liquids or light meals are recommended until you know that you can eat without problems.
Shower
-
You can take a shower tonight – DO NOT WORRY IF THE TUBE GETS WET.
-
After the shower, you should remove the dressing, dry the area and apply a new dressing.
-
You should not soak the wound in water (eg. bath and swimming pool)
